Maeve Boothby O’Neill, a 27-year-old woman from Exeter, England, was too sick to digest food, yet over the course of three separate hospital admissions, she was denied life-saving interventions because medical staff attributed her health issues to deliberate behavior. Instead of giving her the nutrients she needed to live, they considered placing her in a psychiatric facility. In October 2021, O’Neill died of complications from her illness.
As O’Neill wrote to her primary doctor, four months before her death: “I really need help with feeding. I don’t understand why the hospital didn’t do anything for me when I went in. I have been unable to sit up or chew since March. ... Please help me get enough food to live.”
O’Neill’s death has brought attention to the neglected disease from which she suffered, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), undoubtedly one of the most controversial illnesses in the world. The inquest and coroner’s report revealed that not a single doctor at the hospital had any idea how to manage her condition, although it afflicts more than 250,000 people in the United Kingdom and more than 3 million in the United States. As Guardian journalist George Monbiot summed up: “A brilliant and lively young woman with a common illness was repeatedly disbelieved, dismissed and given inappropriate treatment, until she starved to death.”
What happened to O’Neill, I’m afraid, was by no means the exception. We know about her case only because her father, Sean O’Neill, happens to be a senior writer for the Times. “She struggled not just with the debilitating, disabling effects of ME but also with the disbelief, apathy and stigma of the medical profession, the NHS and wider society,” O’Neill wrote in May 2022.
I happen to have the same illness as O’Neill, and the way she was harmed by the very medical system meant to help her is so common with this illness that it’s a trope. After coming down with mononucleosis in my senior year of high school, I ended up developing ME/CFS in my first weeks of college, seemingly overnight, after overexerting myself, like a switch was flipped. In some of my first medical appointments after falling ill, my pediatrician—who had known me for years—looked at me strangely and asked if I was depressed. After some fuss, she referred me to an infectious disease specialist, who told me I had to “deal with my demons.” That was over a decade ago—and except for a short period of remission, my condition has only gotten worse.
ME/CFS is a complex, multi-system chronic illness. It has been recognized by the World Health Organization since 1969 as a neurological disease, and a growing body of biomedical evidence has identified abnormalities in the immune, metabolic, cardiac, and other bodily systems. The condition annihilates energy and ends normal life: The defining feature of the illness is a measurable physiological intolerance to minimal exertion that causes a prolonged exacerbation of all other symptoms, commonly known as a “crash.” There is no FDA-approved treatment or cure, no straightforward lab test to diagnose it, and we don’t know exactly what’s causing it—though it’s likely an immune disorder affecting the nervous system, like multiple sclerosis. It often seems to stem from a viral infection or another immune disruption.
In the absence of standardized care or targeted immunotherapies, the rare practitioner willing to treat ME/CFS as a biomedical condition will generally prescribe pharmaceuticals for specific symptom relief in combination with pacing one’s activities. Counseling and other supportive care may be encouraged, but while therapy may help patients cope, it won’t fix your illness, and exercise has been shown to be harmful for many sufferers. Full recovery is rare, and for many, it is a lifelong and degenerative condition.
We have long known that viral outbreaks leave some minority of the population with long-term symptoms and disability, as we are now seeing with long COVID, which shares many of the same signs and symptoms of ME/CFS: ineradicable exhaustion, brain deficits, post-exertional malaise. Beyond the disabling physical and cognitive issues, it is the medical neglect and disbelief that can hurt—and in some cases kill. Per one 2015 study, patients with ME/CFS have the worst life quality, compared to patients with conditions including long-term mental illness, lung disease, and cancer. Suicide is a relatively common outcome for patients, the suffering so great and hope so dim. A 2024 study from Switzerland found that the disease had a negative mental impact on 88 percent of ME/CFS patients studied, with around 39 percent having suicidal thoughts. And, the authors added, a major factor contributing to those suicidal thoughts was being told the disease was “psychosomatic.”
A major 2015 report by the National Academy of Medicine assessed thousands of studies on ME/CFS and described it as a serious, disabling condition that dramatically impacts the lives of millions of patients around the world. The report stressed that the belief that the illness is “a psychogenic illness or even a figment of the patient’s imagination” is a “misconception,” and it is now acknowledged by major public health agencies in America as a physical disease. And earlier this month, the preliminary findings of a huge genetic study in the U.K. known as DecodeME identified eight regions of the human genome that were substantially altered in patients with ME/CFS compared to those without the illness.
Yet the idea still lingers like a bad odor that it’s “all in your head,” and ME/CFS barely appears in medical training and textbooks. Despite a mountain of evidence and the patient experience itself, a disturbingly large number of medical professionals remain skeptical that the illness even physically exists, an attitude that bleeds into public perception and media. The level of research funding for ME/CFS allocated by the National Institutes of Health—between $10 and $13 million a year as of 2024—is puny in contrast to the disease burden and economic toll, estimated to be in the tens of billions a year from lost wages and medical expenses.
All the headlines around this disease, on the rare occasion they appear, concern the strange gap between how serious and common it is and how little medicine and society seem to know or care about it—“Invisible Disease,” “Forgotten Plague,” “The Most Prevalent Illness You’ve Never Heard Of,” “One of Medicine’s Most Neglected Diseases.”
But how could something so devastating and widespread be so poorly handled and understood?
There have been reported outbreaks of a chronic, flu-like illness with debilitating neurological symptoms all around the world for centuries. But it was first clinically defined in the 1950s following an outbreak at Royal Free Hospital in London, when it was given the name myalgic encephalomyelitis (a medical term for muscle pain and brain and spinal cord inflammation).
When another famous outbreak occurred in Nevada in the mid-’80s, researchers from the Centers for Disease Control (CDC) concluded, after a brief investigation, that it was a nothingburger. The name “myalgic encephalomyelitis” was later changed to “chronic fatigue syndrome,” with the expressed desire to cast doubt on the organic and viral origins of the disease and spare the insurance industry from making excessive payouts, or “chronic disbursements,” as one of the academics behind the name change joked. The logic behind the name change, we know from private correspondence among the naming committee, was that the original name sounded too medical.
The name stuck and made the disease easy to dismiss, diluting a complex affliction to a vague symptom—fatigue—that everyone experiences to some degree. It would soon become stigmatized in media and culture as the “Yuppie Flu”—a fashionable form of upper-class neurosis and hypochondria.
The CDC epidemiologists who were dispatched to study the Nevada outbreak—Gary Holmes and Jon Kaplan—were openly skeptical of the disease in the media, and there were even inside jokes at the agency that included a fake letter on their bulletin board parodying patients as mentally ill hypochondriacs who wanted to get on welfare.
The scandal was brought to light by reporter and patient Hillary Johnson in her 1996 history of the disease, Osler’s Web: Inside the Labyrinth of the Chronic Fatigue Syndrome Epidemic. Johnson’s allegations about the CDC’s mishandling of the Nevada outbreak were definitively confirmed when two separate government investigations unveiled that, throughout the 1990s, the CDC misappropriated tens of millions of dollars specifically allocated by Congress to study this disease and spent it on their own pet projects while repeatedly lying about what they were doing.
Following the course laid by the CDC, a new approach to psychologizing this disease arrived around 1989, known as the “biopsychosocial model.” Some of the creators of this framework, such as U.K. psychiatrists Simon Wessely, Peter White, and Michael Sharpe, played a hand in some of the earliest definitions of chronic fatigue syndrome. The biopsychosocial model has long pushed for non-pharmaceutical interventions for ME/CFS, such as therapies based on the idea that patients are making themselves ill through their beliefs, phobias, and behaviors.
This theory culminated in the controversial PACE Trial for ME/CFS—originally published in The Lancet in 2011 and used to shape treatment guidelines—which purported to prove that patients could recover from the illness with a combination of therapy and exercise designed to break them out of their bad mental and physical habits.
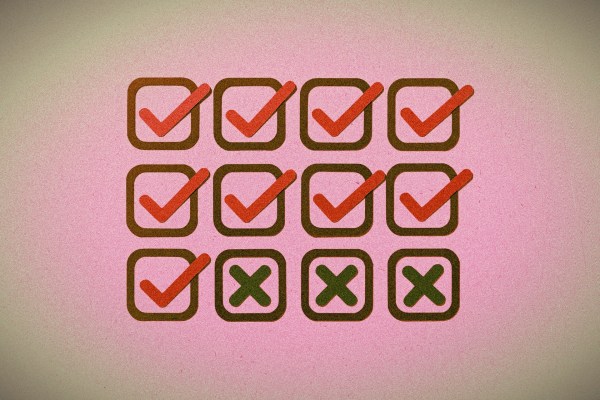
PACE turned out to be a load of bollocks, to steal a term from the Brits, and the study was so ridden with methodological and ethical flaws that it has since been used in college courses as an example of how not to conduct a clinical trial. The main finding of the study contradicted the fundamental patient experience: that exercise makes you worse, not better. Patients doubted the PACE results and launched a multi-year campaign to acquire the underlying data, but their requests were continually denied by the PACE authors until a court ruling forced them to release the raw data—and that raw data did not support the trial’s reported findings.
A comprehensive analysis in 2021 by the U.K’s National Institute for Health and Care Excellence (NICE) found that all of the research promoting cognitive behavioral and graded exercise therapies for ME/CFS were either of “low” or “very low” quality, and major public health organizations like NICE and the CDC have since stopped promoting these therapies to treat ME/CFS.
Yet the PACE authors have refused to acknowledge the flaws of their model and are now applying it to long COVID: Severely ill patients have been placed in psych wards and pressured into exercise programs. The assumption appears to be that patients actually want to be sick, and that any physical condition we don’t fully understand must be caused by the mind.
This has been the story of this disease for decades: one of neglect, patient-blaming, and disdain. As O’Neill’s father put it in a recent interview: “There is a deep cultural resistance in the medical profession to believing that ME is a physical illness.”
The fact is, it’s a challenging and complex disease, and many medical professionals and public health decision-makers appear to have opted for the easier, cheaper, and shorter-term solution—to simply deny the problem exists. “It’s the greatest medical scandal of the century,” wrote George Monbiot in the Guardian in March 2024. “For decades, patients with ME/CFS have been told they can make themselves better by changing their attitudes.”
The mistakes of the past, however, should not determine how we confront problems in the present. Those mistakes have victims, after all—of whom O’Neill is just one example. “I cannot adequately describe how frightening it is to discover there are no doctors who can help you, they do not even know what is wrong with you,” she wrote in January 2021. “I am fighting for a chance to live.”
We cannot let her death be in vain. Without new and improved medicine—and without more collective sympathy—not just for ME/CFS but for all complex chronic illnesses like long COVID, many of us are bound to suffer the same fate as Maeve Boothby O’Neill. The least we owe people with horrifying medical conditions is an earnest, collective effort to mitigate their suffering—and not to deny it exists until they literally die. But for doctors, drug developers, and the public, is the least too much?


Please note that we at The Dispatch hold ourselves, our work, and our commenters to a higher standard than other places on the internet. We welcome comments that foster genuine debate or discussion—including comments critical of us or our work—but responses that include ad hominem attacks on fellow Dispatch members or are intended to stoke fear and anger may be moderated.
With your membership, you only have the ability to comment on The Morning Dispatch articles. Consider upgrading to join the conversation everywhere.