Six months and counting into our coronavirus era, we’ve gotten much better at quantifying the fight against the disease. How well a country or state or county is faring is broken down into charts and scatterplots: Cases per capita and tests run per capita, hospital capacity and PPE availability, test positivity rate and test turnaround rate and case fatality rate.
Given that blizzard of data, it’s strange that one question remains so difficult to examine: How much better are we actually getting at fighting the disease?
We’ve certainly gotten better at fighting the disease’s spread. Everyone knows the drill by now: Masks, social distancing, washing your hands. What’s less obvious is how far we’ve progressed in the task of healing the very sick. Doctors and hospitals have tried to defeat the virus with a cornucopia of drugs and treatments. But in part because that effort has been so improvisational and eclectic, tracking its effectiveness over time remains a serious challenge.
The central fact of the current stage of the pandemic is this: Although new cases soared throughout July and August far above what we saw in April and May, daily COVID deaths have not climbed back to their late-April heights. That rate may continue to rise even with new cases descending again—deaths are, after all, a lagging indicator—but the discrepancy is too sharp to ignore.
But this discrepancy itself does not necessarily indicate improved outcomes in COVID treatment, because other differences between the pandemic’s spring manifestation and its summer one affect the data too. The first wave of the pandemic was clustered primarily in New York and New Jersey, states that failed terribly at keeping the virus, which is most dangerous to the elderly, out of nursing homes. Further, our national testing operation was then in such a sorry state that it’s hard to tell how much viral spread we missed the first time around.
“I think most of the reduction in fatality rate across the country is accounted for by protecting vulnerable populations and by overtesting,” Dr. Howard Forman, a Yale radiologist and health policy professor, told The Dispatch. “So by testing more people who are healthier, we make ourselves look better.”
This certainly isn’t to say there hasn’t been improvement in treating the virus. Clinicians will tell you in no uncertain terms they’ve seen genuine progress. Gone is the desperate chaos of the early months, with their frantic smorgasbord of ad-hoc treatments and what-have-you-got-to-lose therapeutics; now doctors share a sort of anti-COVID folklore, wedding what solid clinical data exists with treatments that their compatriots around the country have found effective from hard experience.
“There’s kind of two parts to the decision-making,” said Dr. Megan Ranney, an emergency physician and professor at Brown University. “Part one, and the part that we are all most comfortable with, is relying on peer-reviewed evidence.” She rattled off a few examples: The antiviral drug remdesivir, which has been shown to reduce COVID’s recovery time; the anti-inflammatory dexamethasone, which can help soothe a berserk immune response to the virus; placing patients who are struggling to breathe on their stomachs rather than their backs.
“The other side is the anecdote, the case series, the shared experiences of groups of physicians,” she said. “This was particularly prominent early in the pandemic when we really had nothing, and no guidance whatsoever. We saw Facebook and WhatsApp groups spring up, as well as email listservs, to try to allow real-time sharing of best practices and to allow people to compare what worked in one setting to what worked in another.”
This loose-cannon treatment style helped doctors begin to catch up to a horribly powerful virus under incredibly bad circumstances, but it had its drawbacks too. Several doctors we spoke to brought up the example of hydroxychloroquine, a drug that showed some early promise in treating COVID patients but was ultimately shown in controlled clinical trials to be unhelpful in treating very sick patients. Ordinarily, that would be the end of the road for a given treatment—but in this case, there were already a number of small case studies and doctors’ personal testimonies floating around with positive assessments of the drug and endorsements from President Donald Trump created a political constituency for its success. Such case studies and anecdotes are inherently less reliable than large-scale clinical trials, but their existence helped fan the flames of the bizarre conspiracy theories that cropped up around the drug.
And it isn’t true that doctors are comfortable now, exactly. It can be hard to remember that we’re still in the very early days of the fight against a brand-new disease. Staying up to date on all the research coming out is a constant struggle of its own. Just this week, for instance, the FDA unexpectedly decided not to issue an emergency authorization for convalescent plasma, a promising treatment involving transfusions of antibody-rich blood serum donated by those who have already had COVID-19, suggesting the data was not yet strong enough to support it.
“I still feel like—maybe not that I’m working in the dark, but that maybe I’m working with one eye closed,” said Dr. Akino Yamashita, who has spent the year treating COVID patients in New Jersey and New York. “Every day, it’s ‘Oh, there’s this new study, there’s this new article.’ … But does [one study] really change what I do when I see the next patient with this disease? Probably not.”
Of the convalescent plasma story, she added: “Certainly this goes along with the theme that although there are more treatment options available now, this is a constantly changing story.”
Nor does the constant churn of new research focus only on better understanding the effects of the treatments already in circulation. Possible new treatments are working their way through the early stages of clinical trials all the time. Antibody treatments, both artificially manufactured and derived from animals, and stem cell therapies featuring cells known as MSCs (which stands, somewhat confusingly, for either “medicinal signaling cells” or “mesenchymal stem cells”)—these are a few of the bleeding-edge projects that could potentially follow hydroxychloroquine and remdesivir into the public consciousness in the months to come.
Of course, this multiplication of possible treatments brings another set of challenges entirely.
“The standard of treatment for a severe COVID-19 illness is changing,” Dr. David Ingbar, a professor of medicine and pulmonary care expert at the University of Minnesota, told The Dispatch. Dr. Ingbar is currently heading up an early clinical trial into treating COVID with MSCs.
“Now we believe dexamethasone works in certain populations at certain levels of illness,” he said. “We know that remdesivir has some benefit in terms of shortening the disease and maybe improving mortality. There are suggestions that, if given early, convalescent plasma might be beneficial. What we don’t know very much about is, how do all of these treatments interact? Is it better to get one from column A, B, C, D, and E? Or are only certain combinations beneficial? So it’s a complicated field, and I think we all as clinicians want to help our patients as much as possible. But there is potential to do harm as well as good with all these treatments.”
Presented like this, all this can seem like a dreary deluge of obstacles and complications. So it’s worth stating unequivocally: All of this is a pretty good problem to have. It may be a while before we can say for sure how far back our medical researchers and clinicians have beaten the virus already. But that fight gets a little less favorable to the virus, and a little more favorable to the humans, every day.
“People forget that the longer you can wait to get COVID—hopefully we’ll get a vaccine quickly, so we’ll be able to protect us all from getting infected—but if you get infected today, your chance of living through that infection is better than if you got infected in February or March,” Dr. Ranney said. “And I expect that to continue to improve. … It’s not a linear process. It’s two steps forward, one step back in terms of that knowledge generation. So there are going to continue to be things that change, there are going to continue to be things that we think help and maybe don’t. That’s normal in medicine. But overall, the trajectory is absolutely a positive and encouraging trajectory in terms of our ability to effectively treat and save lives of patients who are sick with COVID.”
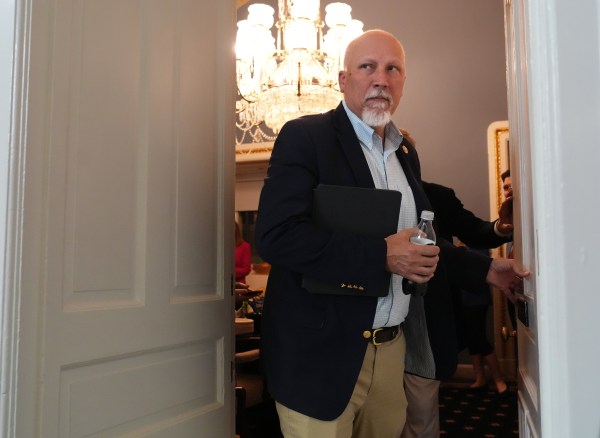
Photograph by Go Nakamura/Getty Images.


Please note that we at The Dispatch hold ourselves, our work, and our commenters to a higher standard than other places on the internet. We welcome comments that foster genuine debate or discussion—including comments critical of us or our work—but responses that include ad hominem attacks on fellow Dispatch members or are intended to stoke fear and anger may be moderated.
With your membership, you only have the ability to comment on The Morning Dispatch articles. Consider upgrading to join the conversation everywhere.