In April 2023, U.S. District Court Judge Matthew Kacsmaryk set off a national media firestorm when he issued a ruling that could—if it ever took effect—threaten nationwide access to mifepristone, one of the drugs taken as part of a two-drug regimen to procure a chemical abortion.
But Kacsmaryk’s nationwide injunction was stayed by the Supreme Court and never took effect. In August 2023, the 5th U.S. Circuit Court of Appeals ruled—in a case described by that court as a “complicated” administrative law appeal—that a legal challenge to the Food and Drug Administration’s (FDA) original approval that allowed the sale of mifepristone in 2000 was barred by the statute of limitations. But the 5th Circuit also held that legal challenges to subsequent FDA actions loosening distribution of the drug in 2016 and 2021 would likely succeed on the grounds that those actions were arbitrary and capricious and therefore unlawful under the Administrative Procedures Act, the law governing how federal executive branch agencies issue regulations.
When the Supreme Court hears oral arguments on Tuesday in the case, FDA v. Alliance for Hippocratic Medicine, it will consider whether the groups of doctors suing the FDA are right that the agency’s 2016 and 2021 deregulatory actions were unlawful. But the original 2000 approval of mifepristone is not even a question before the high court.
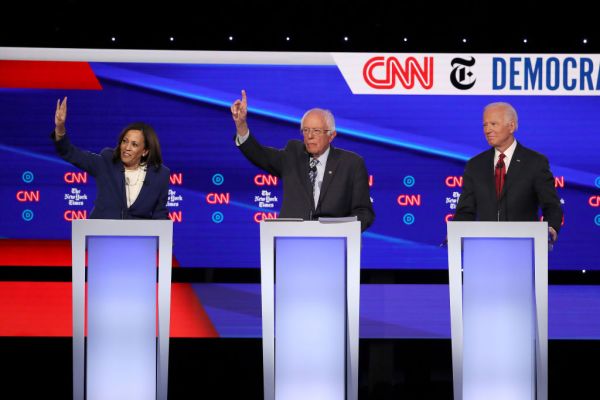
Despite the limited scope of the questions before the Supreme Court, some politicians are exaggerating what’s at stake. Democratic Sen. Mazie Hirono of Hawaii, for example, warned in a recent fundraising email that the Supreme Court could place “access to medication abortion in grave danger.” Of course, if the Supreme Court rules entirely in favor of the doctors challenging the FDA’s actions, it would roll the clock back, perhaps only temporarily, in states where abortion remains legal to the final year of the Obama administration—not exactly a moment in history when anyone considered access to abortion drugs to be “in grave danger.”
What exactly is at stake? When the FDA first allowed mifepristone to be prescribed in the United States in 2000, the agency established several rules to protect women taking it, but most of those rules were eliminated by the FDA in 2016 and 2021. According to the FDA’s 2000 approval memorandum, the pill could be prescribed only during the first seven weeks of pregnancy, and only by a physician who had the ability to “assess the duration of pregnancy accurately … diagnose ectopic pregnancies” and provide or facilitate treatment in cases of serious adverse events.
Three in-person doctor’s visits were also required: first for an examination and taking mifepristone (also known as RU-486), which blocks the hormone progesterone and thus cuts off nutrients essential to sustaining the life of an unborn child. The second visit was to take a separate drug, misoprostol, intended to complete the abortion; and the third visit to ensure there were no complications. The FDA also required the prescriber to “report any hospitalization, transfusion or other serious events.”
All of those rules remained in effect until 2016, the final year of the Obama administration, when the FDA made several changes. The agency allowed the drug to be prescribed during up to 10 weeks of pregnancy and by non-physicians, such as midwives and nurse practitioners. It also removed the requirements that the final two appointments needed to be in person and that prescribers must report non-fatal adverse events. In April 2021, a few months into the Biden administration, the FDA announced it would not enforce the requirement that the first visit needed to be in person, thus allowing the entire process to be conducted remotely. The action allowing distribution of mifepristone without any in-person examination was originally justified by the FDA as a pandemic-related measure, but the agency later made the change permanent on the grounds that risks of taking the pill without any in-person visit to a health care provider was minimal and that telehealth would make abortion more easily obtainable. As the FDA explains in a Q&A about mifepristone, the agency determined in 2021 the rules “must be modified to reduce burden on the health care delivery system and to ensure the benefits of the product outweigh the risks.”
The FDA’s loosening of these rules may have had a significant impact on the number of abortions performed in the United States. The Guttmacher Institute, an abortion advocacy and research organization that was once formally connected to Planned Parenthood, had found abortion rates steadily declining until 2017—the year after the FDA first loosened rules for distributing mifepristone. It recently reported that the increasing trend continued through 2023. Assessing the accuracy of Guttmacher’s estimates is a complicated endeavor, but the organization plausibly cites “broader availability of telehealth for medication abortion” due to the FDA’s 2021 move—as well as increasing public and private funding for abortion, plus blue-state laws becoming even more favorable to abortion rights—as a factor that could have increased the number of abortions in the United States.
In August 2023, the 5th Circuit ruled that the FDA’s 2016 revision ran afoul of the Administrative Procedures Act because the FDA only studied each change individually and not cumulatively. “Because FDA failed to seek data on the cumulative effect, and failed to explain why it did not, its decision to approve the amendments was likely arbitrary and capricious,” the 5th Circuit held. It also ruled that the reasoning for the FDA’s 2021 action—suspending the in-person dispensing requirement—was likely unlawful because it relied on unreliable, self-reported data submitted to the FDA Adverse Event Reporting System (FAERS). “It’s unreasonable for an agency to eliminate a reporting requirement for a thing and then use the resulting absence of data to support its decision,” the 5th Circuit’s opinion read, quoting an earlier ruling by a small panel of the court’s judges.
The doctors suing the FDA argue the rules changes will put more women at risk. For example, an ectopic pregnancy, which typically occurs when an embryo implants in a fallopian tube, is a life-threatening condition if left untreated. It’s usually screened for during an in-person appointment via ultrasound before mifepristone is dispensed. “Patient history simply cannot rule out an ectopic pregnancy. Instead, only an ultrasound can, and it can do so with complete certainty and reliability,” writes Dr. Grazie Pozo Christie, a radiologist, in an amicus brief supporting the Alliance for Hippocratic Medicine. Mifepristone cannot treat an ectopic pregnancy, Christie’s amicus brief observes, and “the symptoms of an ectopic-pregnancy rupture can be indistinguishable from those of a chemical abortion, including dizziness, faintness, bleeding, and abdominal and pelvic pain.”
But the the American College of Obstetricians and Gynecologists (ACOG), which supports abortion rights and the FDA’s actions, argues in its amicus brief that identifying ectopic pregnancy “can be accomplished just as effectively by discussing the patient’s medical history—even via a telemedicine appointment.” To back up that claim, the ACOG brief pointed to a March 2022 study that observed “screening for medication abortion eligibility typically includes ultrasonography or pelvic examination.” But during the COVID pandemic “many clinicians stopped requiring tests before medication abortion and instead screened patients for pregnancy duration and ectopic pregnancy risk by history alone. However, few US-based studies have been conducted on the outcomes and safety of this novel model of care.”
The March 2022 study was conducted under the unusual circumstances of a pandemic from February 2020 to January 2021. Out of about 3,800 women originally included in the study, it only had complete data for roughly 2,400 who took mifepristone without an ultrasound—four of whom had an undetected ectopic pregnancy. The study said that dispensing mifepristone without an ultrasound was safe, but it also noted that “the ectopic pregnancy rate of 2 per 1000 suggests that the screening procedures used by the participating clinics will not triage all patients with ectopic risks to ultrasonography before the abortion. However, the potential benefits of expanded access, increased convenience, and earlier treatment conferred by removing testing requirements may outweigh potential risks of delayed identification of ectopic pregnancies.”
Ultrasound remains a routine part of providing a chemical abortion, even among abortion providers who back the FDA’s rules changes. For example, Planned Parenthood’s websites for patients in states such as New Jersey and Pennsylvania—where the law does not require ultrasounds before an abortion—still list an ultrasound as a standard procedure performed before mifepristone is dispensed.
But the only way the doctors have legal standing to sue the FDA is by establishing that the doctors themselves have been or will imminently be injured. According to the FDA, about one in 25 women will visit an emergency room after taking abortion pills, and the 5th Circuit agreed the pro-life doctors had standing to sue because they had established that “a percentage of women who take mifepristone will suffer serious medical complications; that hundreds of the Medical Organizations’ members are physicians who treat patients in those circumstances; that many of the Doctors have in fact treated such patients; and that providing such treatment causes the Doctors to violate their rights of conscience, sustain mental and emotional distress, divert time and resources away from their ordinary practice, and incur additional liability and insurance costs.” The Supreme Court brief filed by the federal government in defense of the FDA’s 2016 and 2021 actions counters that the doctors’ “central contention is that if mifepristone were available under the pre-2016 conditions rather than the current conditions, the risk that one or more of their members would be called upon to treat a serious adverse event would be reduced to some marginal and unquantified extent. Even if that attenuated, probabilistic injury could satisfy Article III, it would not justify destabilizing nationwide preliminary relief.”
Villanova law professor Michael P. Moreland* told The Dispatch it’s hard to know if the Supreme Court will agree with the 5th Circuit that the doctors have standing. “It’s a close call,” he says. “These standing issues are very technical—they’re very difficult.”
“The court has, over the last several decades, tightened the requirements for standing a considerable amount and said you have to have a kind of particularized cognizable injury that you suffered in order to bring this kind of claim,” he explained.
But oral arguments could provide clues about how the justices might rule—on the issue of standing as well as each of the underlying FDA regulatory changes. “It’ll be interesting to see when the justices get into the questioning how much of it is focused on the standing issues versus the arbitrary capricious issues, how much is as focused on 2016 versus [the 2021] revision,” Moreland said. “If some of the more conservative justices really spend a lot of time on standing and expressing some skepticism about that, then I think that’s probably a very bad omen” for the doctors challenging the FDA.
Either way, said Moreland, oral arguments should “give us some indication of at least where some of the justices are coming down.”
Correction, March 25, 2024: Michael Moreland’s name was originally misspelled on first reference.







Please note that we at The Dispatch hold ourselves, our work, and our commenters to a higher standard than other places on the internet. We welcome comments that foster genuine debate or discussion—including comments critical of us or our work—but responses that include ad hominem attacks on fellow Dispatch members or are intended to stoke fear and anger may be moderated.