A February headline in the Washington Post read, “Mask Mandates didn’t make much difference anyway.” A month later, the New York Times gave us this: “Do Covid restrictions work? Yes, but they didn’t make much of a difference.”
The tone is a bit flippant, isn’t it? It’s as if these headlines are referring to something inconsequential everyone once believed, but later proved untrue. Remember how they used to make us stay out of the pool for an hour after we ate? Turns out that was hooey. LOL!
Maybe it’s wishful flippancy, given the flood of news about the knock-on costs of COVID policies—massive learning losses, an adolescent mental health crisis, a surge in homicides, skyrocketing overdose and alcohol-related deaths, and inflation, to name a few. I imagine many would love to put it all behind us, tucking “COVID Response” on the shelf between “Carrots Don’t Improve Your Vision” and “Cracking Your Knuckles Doesn’t Make Them Bigger.”
The past two years have been far too disruptive and divisive to move on without a backward glance. From what I can see in my own world, even those who earnestly supported and complied with COVID measures have begun to wonder how much of it made sense, or if any of it did.
Like it or not, we’re headed for a National Conversation. If it devolves into endless bickering over masks, school closures, vaccine mandates, or any of the many individual measures that comprised the response, it is sure to be as unproductive as all our other National Conversations.
A more fruitful discussion would begin at a fundamental level, with values and principles we tossed aside, seemingly without scruple, in early 2020.
Some are basic moral principles. Others are foundational to governance and journalism. Some are specific to the practice of public health—perhaps not commonly known, but certainly common sense.
What Were We Doing, Exactly?
“In democratic countries, it’s supposed to be a matter of transparent public debate. What we think our best estimate of the situation is, and the likely outcome of what an intervention might be… a public debate about the appropriate way to proceed that’s as rational and deliberative as possible, and not characterized by fear.” —Dr. Zeb Jamrozik, Infectious disease ethicist, Oxford University, on the Accad and Koka Podcast, September 21, 2021
It’s interesting to look back at the pandemic coverage from late February and early March 2020. Experts who saw what was coming offered fairly gritty prognostications.
According to The Atlantic, we were all “likely to get the Coronavirus.” Harvard epidemiologist Marc Lipsitch said, “I think it’s going to be a new virus that we have to deal with. That won’t be because the United States government has failed to contain it, it will mean that this is an uncontainable virus.”
Anthony Fauci was quoted in the Washington Post saying that once a virus was in multiple countries with sustained transmission, “you could only mitigate it.” There would be no containing it.
A few weeks later, everything was shut down, and we were trying to do just that. What happened in that interval that made us believe we could, and should, contain a supposedly uncontainable virus?
Several things. First, China convinced the world they had done it. As this March 11, 2020, article in STAT reported: “The notion that the curve of this outbreak could be flattened began to gain credence after China took the extraordinary step of locking down tens of millions of people days in advance of the Lunar New Year.”
The author adds: “Many experts at the time said it would have been impossible to slow a rapidly transmitting respiratory infection by effectively shutting down enormous cities—and possibly counterproductive.” (Two years later, tens of millions of Chinese citizens are locked in their homes without enough to eat. Seems “many experts” had a point.)
We also had the images from Lombardy, Italy, and the belief that those scenes would be replicated everywhere if we did not act.
And finally, there was “Report 9” from London’s Imperial College. It is hard to overstate the impact this had on policy: The Simulations Driving the World’s Response to Covid-19 … Behind the Virus Report that Jarred the U.S. and the U.K. to action … The report “helped convince Trump to take coronavirus seriously projected that 2.2 million people could die in the US if we don’t act”… Coronavirus could have caused 40 million deaths if left unchecked.
Professor Neil Ferguson from Imperial College later spoke of having copied China’s model in advocating for lockdowns. “It’s a communist one-party state… We couldn’t get away with it in Europe, we thought… and then Italy did it. And we realized we could.” (“Get away with it”? Um … interesting.)
Again, though, what exactly was it we could supposedly do? We had a slogan—15 days to flatten the curve—but what was the goal? According to Fauci, we were trying to “interfere with the natural flow of the outbreak.” The result would be “less people infected …” to “ultimately have less deaths.” Former FDA Commissioner Scott Gottlieb said a couple of difficult months would allow us to “push down the scope of the epidemic.” Less deaths … Push down the scope.
Fauci and others often said we were only flattening the curve in order to ease pressure on hospitals. That was the message in a widely shared explainer published by Vox. If that was indeed the goal, reducing community transmission of COVID was merely a strategy in service of that goal.
Media coverage, however, hinted at much higher hopes. When New York Times columnist Nick Kristof wrote about a model of “unmitigated spread,” he acknowledged that skeptics “might note that these measures don’t seem to prevent a surge in infections so much as delay them. … There’s something to that: We may see a resurgence whenever we let up.”
“May” see a resurgence. But hey! Maybe not!
Maria Chikina, a University of Pittsburgh computational biologist, and Wes Pegden, a professor of mathematics at Carnegie Mellon, pointed out in this article that “hiding infections in the future is not the same thing as avoiding them.” Once things return to normal, “the epidemic will proceed largely as it would have without mitigations.”
In hindsight, this seems blindingly obvious. A number of comments on the article acknowledged the truth of this, but argued it would buy us time to scale up testing and contact tracing capabilities. By hook or by crook, we were going to control this thing.

By the time states began reopening, it was clear that goal and strategy had become hopelessly conflated. At the end of April, 2020, when Georgia Gov. Brian Kemp rolled back restrictions, The Atlantic published an article titled “Georgia’s Experiment in Human Sacrifice.”
Georgians are now the largely unwilling canaries in an invisible coal mine, sent to find out just how many individuals need to lose their job or their life for a state to work through a plague.
There is much in the article about how reopening would lead to skyrocketing COVID infections. (Cases dropped, by the way.) You know what’s barely mentioned? Hospital capacity.
We were trying to reduce COVID infections, but to what end?
So people won’t die, you homicidal freak!
No one wants people to die (or die prematurely—I must say, I’ve picked up more than a whiff of mortality denial over the past couple of years). But if the virus would just come back, what was the end game? At that point, we did not know if or when we would have a vaccine, and prominent politicians vowed they would not trust it if we did.
At the end of 2020, Vox wrote a follow-up to its “flatten the curve to save hospital capacity” explainer. It was “evident that trying to flatten the curve was not sufficient to end the pandemic.”
Oh. So … we were trying to end the pandemic?
Well, manna from heaven: Soon we did have a vaccine. Proponents of extended COVID restrictions could finally complete the sentence: “Reduce transmission … until people are vaccinated.”
Except that didn’t do the trick either, did it? The vaccines do not prevent transmission, and even when we thought they did, a vocal segment remained adamantly opposed to lifting what restrictions remained. Without a clear goal, we were stuck in “reduce transmission until _______?”
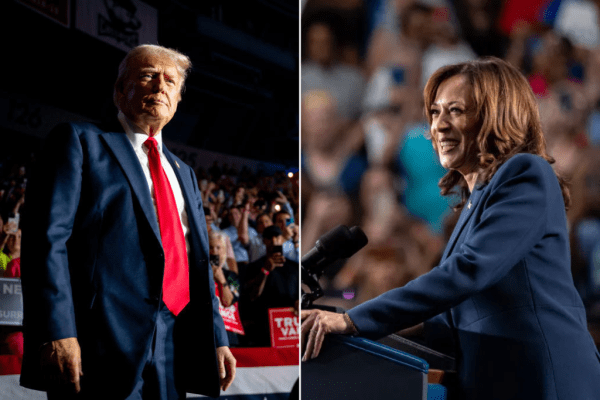
It was only after the off-year elections in Virginia and New Jersey, which portended big losses for Democrats in the coming midterms, that blue states began to loosen their grip on restrictions. A number of prominent experts still insist they should remain in place.
All along, “Zero COVID” advocates have been thick on the ground. COVID meets virtually none of the criteria for a virus that could be eliminated, but that hasn’t stopped the But Smallpox! comments. “You are either with the virus or against the virus; there is no middle ground,” Soledad O’Brien tweeted in January. When asked what victory would look like, she replied: “See Polio for a reference.” (Never mind that, among other differences, polio isn’t airborne and has no animal reservoirs.)
Suppose public health and elected officials had stuck with the original prognostications: Eventually, we would all encounter COVID. There was no containing a highly contagious respiratory virus, which many people carry asymptomatically. All we could do was mitigate the harm while we waited for herd immunity, whether it came from natural infection, a vaccine, or both.
What if, instead of being guided by mathematical models, we had stuck with more concrete knowledge? Pandemic planning guides were sitting on the shelf, waiting to be consulted, and were far more deserving of the label “The Science™” than epidemiological models.
As this article points out, studying similar past pandemics would also have been a better guide: “Every established respiratory pandemic of the last 130 years has caused seasonal waves of infection and has culminated in viral endemicity.” Models, however, “excluded this possibility through the failure to incorporate seasonal transmission effects, or either pre-existing or partial post-infection immunity to infection.”
The impulse to find a scapegoat has been a feature of epidemics for thousands of years, so I suppose it’s not surprising how quickly COVID morphed into one of our modern morality plays, in which politics stand in for religion. This was largely due to mismanaged expectations, the tantalizing possibility that we could “beat” COVID, that it was just a matter of national will and selflessness.
Had public health and elected officials been more realistic, would we have obsessively compared the “performance” of various states and countries—comparisons that eventually looked foolish, when the supposedly “good” state or country got hit, as all inevitably did?
I’m not sure. I only know that we spent a good part of the past two years trying to “crush the virus” by “following the science.” And that no one ever really knew what that meant.
Empiric Interventions
“Valuable financial and personnel resources are used in the development and implementation of public health policies and plans. Therefore, care should be exercised in ensuring that the bases of such policies and plans have been rigorously tested and proven viable.” —American Public Health Association Code of Ethics
In May 2020, Scott Gottlieb appeared on CBS News’ Face the Nation. “While mitigation didn’t fail, I think it’s fair to say that it didn’t work as we expected … We expected to see more significant declines in new cases and deaths around the nation at this point and we’re just not seeing that.”
If an approach—untested, and extraordinarily disruptive and expensive—is not meeting expectations, is that not a good time to question the assumptions behind those expectations?
Nah.
Crises are scary, and solutions are often opaque at first. There will be some grasping at straws, wild overspending, plenty of wrong turns. If you end up doing roughly the right things, and the only issue is the scale of the cost, that’s just how it is.
With COVID policies, it was not just a question of scale. In addition to a vague, unachievable overarching goal, there was also unshakable belief in the various mitigation measures that comprised the response, an unwillingness to articulate what, precisely, each was meant to achieve, or to weigh benefit against cost. And while many of these measures had little to no empiric foundation, there was stubborn resistance to testing their efficacy.

Especially in deep blue areas, any restriction or mandate instantly became the status quo, the null hypothesis: The Science™. It was like the children’s game King of the Hill. Rolling back any policy required proving that doing so would lead to no community transmission of COVID. Fail to prove a negative? Back down the hill you go.
In defending measures, COVID maximalists often invoked the Precautionary Principle, sometimes known as the “better safe than sorry” rule. This was a one-way reading of the Precautionary Principle, and some would say a backward one. The standard interpretation of the Precautionary Principle biases the status quo—not “restriction as status quo,” the original status quo. It is meant to be a backstop against hasty implementation of policies that might cause harm, and places the burden on advocates for an intervention to prove it will not do so. (Importantly, the Precautionary Principle has always given special consideration to any action where children might be affected.)
In an emergency, it might make sense to try an intervention while data is gathered … but the data must be gathered! The reluctance to provide robust evidence for COVID policies contributed to decreased trust in public health authorities, and likely prevented energy and resources being devoted to the highest-yield efforts.
Randomized cluster control trials can be designed for almost any intervention, and results can help clarify what a particular policy will achieve. For example: “X toddlers wearing cloth masks will prevent one COVID hospitalization.” (Actually, that one’s easy: X=infinity, because cloth masks don’t work.)
The freakout over the ruling about airline mask mandates is a perfect illustration of the kind of battle that might have been averted with better data. The mandate allowed any kind of mask, and removal while eating and drinking. People tend to fill in gaps in data with instincts or personal beliefs, but “every little bit helps” is not a data-driven rationale for a policy. The fact is, the medical world is littered with examples of interventions that make intuitive, mechanistic sense, but which utterly fail when subjected to rigorous testing. Many COVID policies failed to even meet the threshold of making mechanistic sense (grocery store floor arrows, anyone?)
As Jonathan Chait said, progressives “were carried along by … a zero-COVID policy that refused to weight the trade-off of any measure that could even plausibly claim to suppress the pandemic.”
The problem, of course, was that the COVID response had been hopelessly grafted onto our politics. We had “Team Taking COVID Seriously”—believers in The Science—engaged in a noble battle against “Deniers” and “Minimizers.”
Full-throated support of COVID mitigation measures signaled caring about one’s community. Any skepticism was equated with selfishness. Wearing a mask, staying home, believing The Science™—that wasn’t what you did. It was who you were. Advocates for endless COVID policies frequently seemed, as Josh Barro put it, more concerned “about how we should regard COVID than how we should prevent it.”
There was no room for those who were rationally concerned about COVID, but also about the response. Questioning COVID policies was tantamount to donning an enemy uniform—or, at best, labeling oneself a collaborator, aiding and abetting a dangerous enemy. Do you know who retweets you when you say schools should open? Deniers, that’s who!
Smart, dumb. Good, bad. Life, death. All the elements of our toxic partisan discourse, with all its tired, reductive, false dichotomies.
As two Rutgers law professors said in this excellent essay in Tablet, discourse was “fostered by an elite culture whose overconfidence led to … undermining open discussion in a vain attempt to prove that complex questions could only have one universal and immutable answer.” The “overselling of policy … led them to religiouslike zeal and dogmatism about particular interventions.”
The faith in COVID policies was so entrenched, lack of compliance was the only conceivable explanation for our failure to crush the virus. A constant refrain on Twitter was, “The only reason X doesn’t work is because people won’t [thing they won’t do].”
That’s not true, as it happens, but even if it were, only two words in that sentence matter: “doesn’t work.” Those tweets might as well have said “X is the wrong intervention.” Why? Because people won’t do it. It really is that simple.
A basic principle of public health is that interventions must work in our world, as it is, with the people who live in it. If people are rotten and selfish, as many seem to believe, then the approach must be designed to work in our rotten and selfish world. No points for being “right” on paper (or Twitter, or cable news).
The New York Times’ assertion that COVID restrictions “work” but didn’t make much of a difference was likely fan service, an attempt to placate readers deeply devoted to these policies. (They were furious anyway.) It was wrong, though. Public funds, patience, trust, and attention are precious commodities that should not be squandered on low- or no-yield interventions.
As Dr. Stefan Baral, a practicing physician and professor of epidemiology at Johns Hopkins, tweeted, “Public health is a service industry. Similar to other service industries, the customer is always right.”
‘Germalism’
I recently read up on the swine flu (H1N1) pandemic in 2009. The relevant federal agencies performed relatively well, thanks in part to a much clearer delineation of roles. The CDC led the public health response. NIH (NIAID, specifically) oversaw vaccine development. The White House mostly stayed out of the way.
A great deal of mischief, I’m afraid, flowed from the White House NOT staying out of the way this time around. COVID briefings at the White House, covered by the political press corps, triggered “Newton’s Third Law of Trump”: The “equal and opposite reaction” dictates that whoever opposes Trump must be as right as Trump is wrong.
Never, not for one second, did it occur to me to listen to Donald Trump about COVID. But more than one person can be wrong at the same time.
Journalists are supposed to be wary of sudden, massive expansions of government power. With COVID, we had the government hemorrhaging money, impeding civil liberties, and causing untold harms. All the while, officials were opaque about goals, metrics, outcomes, evidence, and knock-on costs. And starting on Day 16 of “15 days to flatten the curve,” the effort was failing on its own terms.
This was a prime chance to “speak truth to power,” but rather than exhibiting skepticism about these policies, most of the media joined the chorus demanding them, with criticism reserved for officials they deemed insufficiently aggressive.
We needed journalism, but what we got was “germalism”: the media, experts, and policymakers in an endless feedback loop of single-factor analysis. Anyone who questioned policies was the enemy, and could be given no quarter.
Alarmism is a media incentive in the best of times. Now it was also a virtue, perceived to be a vital counterweight to the influence of the enemy, who were endangering lives by relaxing measures, or expressing optimistic views that could discourage vigilance.
Refusal to countenance doubt about the efficacy of policies, or even any suggestion that forces besides human behavior might affect the trajectory of the pandemic, led to absurd journalistic contortions.
When less restrictive red states or regions were hit hard, the governors were killing citizens. If things were all right, citizens were following recommendations anyway, because they knew what was best. (Until things went badly, a clear sign they had Let Their Guards Down). There might be a brief nod to seasonality when a wave moved north, but amnesia would quickly set in when a wave hit the south again.
Sweden bucked the lockdown trend, and when outcomes were not as dire as predicted, it triggered the “nearest neighbor rule”: Sweden could be compared only to Norway and Finland. Meanwhile, it was perfectly kosher to compare the United States to New Zealand. Most of what’s been written about Sweden, by the way, is wrong, or at a minimum incomplete. Though characterized as radical, Sweden took a fairly textbook approach—albeit more nuanced than is commonly understood—which is becoming harder to demonize as longer-term data emerge.
The media is not entirely responsible for the groupthink on COVID. Epistemic closure and stifling of debate in the scientific community, particularly among elite academics, played a major role. But it’s not a stretch to say that the hive mind could not have formed had the media not treated expert opinion as received truth, The Science™.
Benefit and Burden
On a recent podcast, infectious disease ethicist Dr. Zeb Jamrozik pointed out that decision making in an epidemic should not be dictated solely by the output of epidemiological models. Public health should be guided by core ethical principles. These include proportionality, equity, fairness, reciprocity, transparency, and the use of the least harmful policies. (Okay, so: no, no, no, no, and no.)
Importantly, officials must not only identify “what the aggregate effect of public health benefit or harm is expected to be for a given set of interventions, but what the distribution of those benefits and harms is going to be.”
On this, we saw a clear failure. Elites enjoyed the benefits, while our most vulnerable were saddled with the harms.
Children and the Burden of Restrictions
On April 13, 2020, Bethany Mandel tweeted a thread that began with the following:
She went on to list various sacrifices children were making, and closed with a question: “At what point do we say that their lives have to be factored into this conversation?” Pre-2020, the answer would have been “before we imposed any restrictions.”
We don’t ask children to protect adults. We just don’t. In a million years, I would not have imagined that being a controversial statement. In the U.S., as in every society in the world, policymaking has always given weight to the protection and interests of children. Yet here we are.
The fusillade of rage that followed Bethany’s thread showed just how far and fast the Overton window had moved:
“Your children’s real sacrifice is having a sociopath for a mother” … “Imagine growing up knowing you brought home a virus that killed someone who nurtured and loved you” … “This is a good opportunity to teach kids that the world is not all about them, particularly since I’m guessing that it’s also difficult to explain why grandma’s not coming back …”
“What could it hurt?” should not be a rhetorical question. It is a moral good to care about the anonymous, vulnerable person down a chain of transmission. However, it is also a moral good to care about the anonymous, vulnerable person who is harmed by COVID mitigation measures.
When media and elected officials are hyperfocused on the former, and any mention of the latter is treated with scorn, grave harms can result. This is precisely what occurred.
Parents voiced little objection when schools closed in spring 2020. Like most Americans, they were willing and eager to do all that public health officials asked of them. Even when 15 days turned to several weeks, then months, and more than a year in many places, there was remarkably little objection.
“Schools are open” has always been the default condition. Pandemic plans contemplating viruses particularly deadly to children did not recommend extended school closures. In many parts of the country, however, parents learned that the reward for their sacrifice was remote school as the new default condition. Another game of King of the Hill, requiring parents to battle elected officials, teachers’ unions, media, and the very public health officials for whom they graciously made this sacrifice in the first place.

As we know, many parents have awakened to this betrayal. (As the mother of a student in the high school class of 2020, I can attest that young people too are increasingly aware they were victims of a massive bait and switch.)
Some parents did support school closures, having been frightened by anecdotes and uncontextualized data from media and the more alarmist of our newly minted expert class. Fauci got into the action, with periodic reminders that “some children do get seriously ill.” True, but that was the case with other contagious illnesses for which schools never closed.
Alarmism about kids’ COVID risk is on the rise again, as COVID maximalists fight one of their last battles, masks on toddlers (possibly the weirdest hill to die on in the history of hills to die on). Throughout most of the pandemic, however, few pretended that children were the object of concern in our policies. Remember the great school reopening debates of Fall 2020? Those were centered entirely on the extent to which schools contributed to community transmission of COVID. In other words: children protecting adults.
School closures, remote learning, toddlers in masks, cancellation of activities, and the effort to terrify parents were all in service of the strategy: reducing COVID transmission through broad, population-wide restrictions.
Children were at the least risk from COVID, yet we forced them to bear the greatest burden of restrictions.
Essential Workers and the Burden of Disease
“During implementation of public health laws, regulatory bodies should use scarce resources efficiently to produce just outcomes, with a fair and equitable distribution of resources.”—American Public Health Association Code of Ethics
COVID discourse, particularly on Twitter, was characterized by blaming, shaming, and moralizing. With Omicron, we were treated to the “I did everything right, and I still got COVID” threads, one of the most tedious genres on that tedious platform. (Click here for the best sendup of the category, and here for the magazine-length version, wherein a 39-year-old endurance athlete gets COVID, coughs 20 times, and has an existential crisis.)
Chris Cillizza said the quiet part out loud in a January thread. When the Omicron wave hit, he learned that many people had already had COVID, but had not previously admitted it, suggesting they had been embarrassed. “I do think societally we unknowingly turned having COVID into a judgment on your character,” he mused.
You don’t say!
I appreciated his candor, glad he finally recognized what had long been incandescently clear to many: Elites believed that people who did the right things would not get COVID. The implication, of course, was that those who did get COVID should feel ashamed, having clearly done the wrong things.
From their obsessions and observations, it was obvious elites were viewing the pandemic mostly through their computer. (Or, occasionally, out their windows: We’d have crushed this virus already, if not for that maskless guy out there by himself, walking his labradoodle!)
After two years of scanning for sins—from people gathered outside on beaches in 2020, to college football fans rushing the field in late 2021—this was “the view from the elite bubble,” completely detached from the reality on the ground. And deeply ironic, given that those of us who had the luxury of working from home had simply offloaded our risk.
It might feel virtuous to order a meal from DoorDash, but someone had to make that meal, and that someone is likely at greater risk than whoever ordered it.
Epidemiological models are good for testing hypotheses, and in that limited way can be useful for crafting policy. However, they are blunt, simplistic instruments that mostly assume homogeneous risk. In reality, we all have different risks of contracting COVID, of onward transmission, and of severity of disease.
Broad, restrictions-based interventions that epidemiologists modeled, and much of the west adopted, often have the effect of concentrating epidemics, making them more difficult to control.
Risk factors are not rocket science. Someone living in a multigenerational household with one or more essential workers, and fewer than one room per person, is at a higher risk of contracting and transmitting COVID, potentially to someone at risk of a bad outcome.
Unsurprisingly, the highest COVID case rates and worst outcomes were consistently in low-income zip codes, home to many of the people who kept grocery stores stocked and restaurant kitchens running, and who packed up and delivered all that was needed by the virtuously, voluntarily home-bound.
In addition to balancing the overall burden and benefit, public health interventions should do more for those who need more. The blunt, top-down approach gave elites a comforting feeling of control and protection (and, evidently, of accomplishment), but it put the greatest burden on our most vulnerable, and likely made the epidemic worse.
That’s what we should be ashamed of.
Public Health Expertise
The fact is, in designing our COVID policies, we deferred to the judgment of experts who were not qualified.
Don’t get me wrong: I’m sure many of the disease experts and others who freely gave of their time and wisdom deserve our gratitude. Most are probably quite brilliant at what they do.
It’s just that we asked them to do something else.
To borrow from photography, public policy generally—and public health specifically—requires a wide-angle lens. Policymakers must weigh many competing societal needs, and public health officials must consider the broad spectrum of human wellness and flourishing.
Experts in certain fields were understandably single-minded in their focus on COVID. When it came to fitting COVID policy into a broader context, however, they were simply out of their lanes. It’s not their fault. It’s the job of policymakers to listen to voices from a variety of fields, and balance their constituents’ varying needs. (Though it would have been helpful had the experts, and the media who elevated them, acknowledged the limits of their expertise).
It’s also important to note that, while many prominent experts fall under the general umbrella of “public health,” few are actual public health practitioners.
Public health includes many areas of specialty—disease experts, epidemiologists, specialists in informatics and data management, and more. Designing and implementing interventions, the job of public health practitioners, requires a separate skill set from that of epidemiologists or mathematical modelers.
Public health practitioners are well-represented in state and local governments, but less so at the national level and in academia. Most prominent, visible COVID experts hailed from the federal government and universities. They tend to be more partisan, and more sympathetic to technocratic solutions. Their marvelous certitude, along with an ability to appeal to partisan priors, slotted neatly into our political COVID discourse.
Expert tweet: We must all do X to crush the virus!
Virus: [not crushed]
Expert tweet: THOSE SELFISH PEOPLE wouldn’t do X!
No wonder politicians, especially in blue states, were so enthusiastic about arbitrary COVID restrictions. They could simply flip a switch, shut things down hard and fast, and they were showered with praise for Doing Something.
Unfortunately, these blanket restrictions were never destined to have a meaningful impact on mortality. It’s intuitively appealing, the idea that we should mandate a behavior if we believe it will yield a desired health outcome. But it’s simply not true.
Public health practitioners tend to favor “resources before restrictions.” A story Dr. Stefan Baral told on Bari Weiss’ Honestly podcast explains why. When COVID hit, he put together an isolation plan for the Toronto homeless shelter where he provides clinical services. Early in the pandemic, he often received calls from hospitals, asking if he had room for COVID patients who were not sick enough to stay in the hospital but had no place to shelter safely.
He didn’t. So, where did they go? Home, to their crowded, multigenerational households. A perfect illustration of what the Zoomocracy failed to understand: So often, the problem was not what people wouldn’t do, but what they couldn’t. In this case, isolate.
Public health practitioners, for pennies on the dollar, could have targeted resources to meet actual needs, mitigate actual risks. Their work is context specific, and doesn’t fit neatly into 280-character tweets, but a few examples: They might have paired positive tests with offers of hotel vouchers for people whose living situations do not permit them to isolate. Or created a pool of resources for workers who do not have paid, or even unpaid, sick leave. Or figured out a way to help nursing home workers who move from job to job, and live paycheck to paycheck.
The initial appeal of top-down restrictions was understandable. It seemed so simple, so tidy. Its advocates had wonderful educational pedigrees and spoke with such comforting authority. It was hard to swap out their theoretically leak-proof solution for a more practical approach.
The failure was in refusing to recognize that the supposedly simple solution was quite leaky, indeed, and that all the angry tweets in the world could not patch it up.
Engagement and Honesty in Public Health
The American Public Health Association’s Code of Ethics points to how public health communications during COVID failed to meet ethical standards.
Policies, the APHA points out, are “most effective when community members participate in their development.” That’s why, in addition to resources over restrictions, public health practitioners favor recommendations over mandates.
Straightforward, honest, transparent communication is critical, because “honesty and accuracy build public trust, which is essential for the success of most public health efforts. … Being honest and accurate in communications with the public also demonstrates respect for the individuals and communities that public health serves.”
Blaming, shaming and point scoring are great for pushing political outrage buttons, but they’re alienating in public health practice, where you deal with real people, not caricatures on Twitter. Effective public health prioritizes “respect for the dignity and capability of individuals, not on strategies of stigmatization or on appeals to motivations of fear, disgust, and shame.”
As to the use of fear to motivate behavior, the APHA suggests communicating about risk “in a variety of ways (e.g., absolute vs. relative) to avoid overemphasizing or underemphasizing potential harm.”
As this article points out, those who use scare tactics often assume that individual behavior is driven primarily by fear (or lack thereof), rather than circumstances, a view shared by many COVID experts, as well as by our tech overlords. Censorship of COVID “misinformation” never extended to alarmist statements, no matter how false. If you believe we aren’t “crushing the virus” because people aren’t Taking COVID Seriously, why not ratchet up the fear to change their minds?
In reality, surveys consistently showed that people had wildly outsized perceptions of their personal risk from COVID. This, in and of itself, is not without consequences. Living in fear for protracted periods of time can cause chronic health conditions, as outlined in this thread about the U.K.’s “nudge unit,” which “deliberately stoked fear in the physically well to protect the physically vulnerable.” (The vulnerable were already protecting themselves—further evidence of the efficacy of recommendations over mandates.)
I look forward to someone studying this more thoroughly, but in my observation, alarmism made the anxious more anxious, annoyed the “rationally concerned” (a category to which I belong, but which our dichotomous partisan discourse insisted did not exist), and, I suspect, made the “irrationally unconcerned” more skeptical.
Exaggerated risk perceptions also served to keep dubious interventions in place for far too long. We have only begun to calculate the damage wrought by these interventions. Some imagined harms might not come to be, but others, as yet unimagined, will surely emerge. It is inevitable, given the institutional and media resistance to weighing costs and benefits.
What Next?
Remember those In/Out lists we used to see around December 31 every year? Maybe we need one for an after-action review of COVID.
Out: angry dogmatism.
In: epistemic humility.
Out: solving for COVID, and only for COVID.
In: recognition that public health is about more than one contagious respiratory virus.
Out: children as vectors of infection.
In: prioritization of the interests and well-being of children.
Out: The Science™.
In: Science as a process.
Pre-2020 pandemic preparedness plans, written by cooler and wiser heads, share some common themes. They are grounded in reality, and account for and accept human needs and tendencies. Implicit in all of them is an understanding that other things matter, that other things must matter.
In March of 2020, an elite consensus formed that nothing mattered more than the effort to reduce transmission of COVID. A child could be locked in a home with an abusive parent. Loved ones could be left to die alone. Other deadly diseases could progress, undiagnosed and untreated, because no death was as tragic as a COVID death.
What is so vital to human beings, one of the most social species on the planet, was deemed unnecessary—sinful, even. We were told that the best way to fight COVID—indeed, the only way—was for all of us, at all times, to behave as if we were infected, and infectious. This was, by definition, almost never true, but society had to be reordered, other human needs sacrificed, in order for us to pretend it was.
Treating ourselves and others as little more than potential vectors of infection (a phrase that, sadly, was most commonly used to describe children) was an astonishing assault on human dignity. I suppose it is somewhat comprehensible through the lens of the early promise that we could “crush the virus.” But after fifteen days, why did it continue?
I imagine people will be chewing on that question for decades. Our great grandchildren will probably read cogent arguments in history books that tie the COVID response back to the 2008 financial crisis, or 9/11, or the assassination of Archduke Franz Ferdinand.
In the meantime, though, we need an honest discussion about how we proceed from here, and it must be free of the bullying, dogmatism, and bad faith exhibited by many experts over the past two years. The Science™ has held up poorly and will likely crumble further as time goes on, but that will not stop defenders of COVID policies from insisting it was all worthwhile.
That question—was it worthwhile?—cannot be answered by numbers, no matter how they are sliced and diced. We had a social contract before COVID hit. Like all social contracts, it emerged organically over time, and perhaps it needed to be revisited. But there was no such debate in 2020. The contract was simply tossed overboard, along with the values and principles underscoring it. Any suggestion that this was perhaps a bit precipitous was deemed morally reprehensible.
For this reason, discussion over what to do if, God forbid, we face another pandemic, cannot use the COVID response as the baseline.
Where, then, should such a debate begin? I’d suggest the following:
Out: Nothing else matters.
In: Other things matter. Other things must matter.






Please note that we at The Dispatch hold ourselves, our work, and our commenters to a higher standard than other places on the internet. We welcome comments that foster genuine debate or discussion—including comments critical of us or our work—but responses that include ad hominem attacks on fellow Dispatch members or are intended to stoke fear and anger may be moderated.