It’s been just longer than two weeks since the first batches of Pfizer’s COVID-19 vaccine began rolling out nationwide, and 10 days since Moderna’s did the same. According to CDC data, a combined 12,409,050 doses of these two vaccines—both of which were developed and received FDA authorization in less than a year—have been distributed across the country, and 2,794,588 of those doses have been administered.
In a vacuum, inoculating nearly 3 million people against a deadly virus less than a year after it was sequenced is nothing short of a miracle. But given that the daily death toll in the U.S. has averaged nearly 2,500 this month, some are saying it’s not good enough.
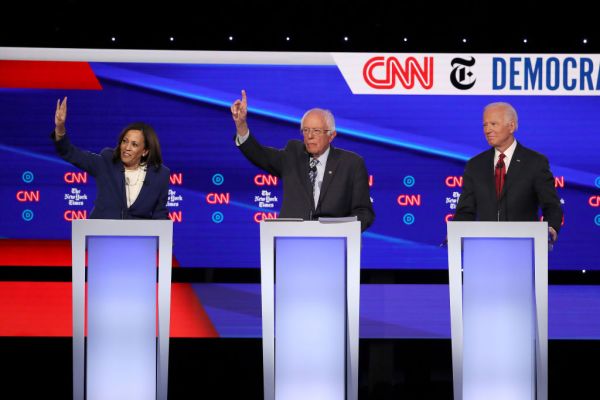
“The Trump administration’s plan to distribute vaccines is falling behind,” President-elect Joe Biden said on Tuesday. “We are grateful to the companies, the doctors, the scientists, the researchers, the clinical trial participants, and Operation Warp Speed for developing the vaccines quickly. But as I long feared and warned, the effort to distribute and administer the vaccine is not progressing as it should.”
Biden referenced Operation Warp Speed chief Moncef Slaoui’s suggestion that 20 million Americans would be vaccinated by the end of the year, pointing to the CDC’s relatively meager 2.7 million figure. “At the pace the vaccination program is moving now,” he said, “it’s going to take years, not months, to vaccinate the American people.”
The pace, of course, will pick up as infrastructure continues to be built out and additional vaccine candidates are authorized. But Biden’s speech did tap into a legitimate concern: If 12.5 million vaccine doses have been distributed around the country, why have fewer than 3 million people received one?
The answer, like just about anything having to do with the COVID-19 pandemic, is complicated.
First of all, reporting delays across the country make the gulf seem wider than it is. Gen. Gustave Perna, the chief operating officer of Operation Warp Speed, told reporters yesterday that he is seeing a 72- to 96-hour lag in the CDC’s dashboard. “That data will tighten up as systems and reporting become more regular and routine,” he said.
This is not the first time the CDC’s data processes have been under the microscope. “Federal coordination about data collection has been horrible,” Dr. Howard Forman, a health policy professor at Yale University and clinician at Yale New Haven Hospital, told The Dispatch. “It’s why there is a COVID Tracking Project run out of The Atlantic magazine, because the federal government never wanted to take on the responsibility or even work directly with groups to try to quickly collect this type of information.”
By implementing universal and consistent vaccination reporting guidelines, Forman added, the federal government could have avoided this confusion, which he believes has led to the undercounting of vaccinations administered. “There’s no great incentive for a state or a health system or anyone to report back right away,” he said. “There’s nothing in it for them, and there’s nobody making it easy for them. So I’m sure they’re collecting the data, but it’s probably not even close to real time.”
Even accounting for reporting delays, top Operation Warp Speed officials have conceded progress isn’t as far along as they’d like. “There is a lag in how the numbers are computed, but surely it’s a number that is smaller than the 14 million doses that are out there already available for use,” Slaoui said yesterday. “We agree that that number is lower than what we hoped for. … We know that it should be better, and we’re working hard to make it better.”
“Of course, we need to be doing a better job,” Health and Human Services Assistant Secretary for Health Adm. Brett Giroir added. “But all vaccine programs start somewhat slow. … We had two holidays and three snowstorms. But I think it’s more of just you starting a program, and that starts relatively slowly and ramps up very quickly.”
The myriad causes for this slow start become apparent in talking to those actually administering the vaccine. “The holiday season has certainly slowed down the rollout,” said Dr. Akino Yamashita, who is treating COVID patients in New York. “The hospital I work at is providing vaccines to staff, but only on weekdays. There was also a snowstorm in the Northeast that slowed some shipments and forced some places to close early the day of the storm, or open later the day after.”
The Pfizer vaccine’s extreme temperature requirements may also be contributing to the relatively lethargic uptake, Yamashita noted. “Once you defrost them, you can keep the vaccine in the fridge for five days,” she explained. “Once you take it out of the fridge and prep it, you have six hours to give it. If not, you have to throw it out. I think some centers might be limiting vaccination hours because they don’t want to wind up with wasted vaccines if people don’t show up.” Aurora Medical Center outside of Milwaukee had to dispose of more than 500 vaccine doses earlier this week after an employee left them out overnight.
The sheer novelty of the vaccine presents another administration bottleneck, as CDC guidelines recommend doctors and nurses keep recipients on the premises for 15 or 30 minutes post-vaccination, depending on their medical histories, to monitor for any side effects or allergic reactions. STAT News reported earlier this week there have been 11 U.S. cases of post-COVID vaccine anaphylaxis—which can be treated with an EpiPen—out of about 2.1 million doses administered. As pediatrician Aaron Carroll wrote this week in the New York Times, the COVID-19 anaphylaxis rate thus far is slightly higher than the overall rate of anaphylaxis in vaccinations, “but that may be only because we are being much more careful about monitoring reactions at the moment.”
Forman, who had vaccinated about 45 people yesterday by the time The Dispatch caught up with him in the afternoon, said his health system hadn’t seen any severe reactions after administering “well over” 10,000 inoculations. But in a pandemic, the extra 15- to 30-minute wait time is particularly disruptive. “People are filling up our room, socially distancing, after the vaccination,” he said. “Which means that even if you wanted to schedule twice as many [vaccine appointments], where would you hold them?”
“I hope that in the next two or three weeks the CDC will change their guidance and say, ‘You know what? Most people are capable of monitoring themselves,’” Forman added. “As long as they don’t leave the campus, they can walk around, they can go toward their car. … Things like that actually would change the number of [vaccinations] that we could schedule in a given amount of time.”
Doses and physical space aren’t the only vaccination components hospitals and clinics are running short on: They also need trained professionals to administer the shots.
“My hospital has such a degree of burnout from the two COVID waves,” Forman said, noting that simultaneous surges across the country mean health systems can no longer call in reinforcements from elsewhere in the country. Plus, with nationwide COVID hospitalizations setting record highs essentially every day, treating the currently sick patients remains the top priority.
“There’s a lot of strain on the system now. Put on top of that, you have a holiday time. People have basically been forced to work through their vacations throughout the previous part of the year. And so you have a shortage of people able to do the vaccines in clinics,” Forman said, adding that he and everyone administering vaccinations with him yesterday was doing so on a volunteer basis and on their own time.
The massive coronavirus relief package passed by Congress earlier this month appropriated nearly $30 billion for vaccine purchases and distribution. Additional vaccine candidates from AstraZeneca, Novavax, and Johnson & Johnson could receive FDA authorization in the coming months. Both developments will play a large role in the United States reaching herd immunity.
Slaoui was asked yesterday if this longer than expected ramp-up phase has affected his previous expectation that the broader population will be getting vaccinated by April. “In terms of vaccine doses, available, manufactured, approved for use, there is no reason to believe there would be any change,” he said. “We have planned 20 million doses by the end of the year, they are there; our plans continue to be the same. I have each time cautioned that manufacturing a vaccine is very complex and therefore at some point there could be hiccups. But there’s none at this stage.”
The administration is adamant that it has hit its end-of-year goal: While 20 million vaccine doses won’t be administered by Thursday night, they will have been allocated.
“Operation Warp Speed has approximately 40 million doses of vaccine by the end of the year and, as of Tuesday, has allocated 20 million doses for first vaccinations, with distribution of the 20 million first doses spanning into the first week of January as states place orders for them,” Operation Warp Speed spokesman Michael Pratt told The Dispatch yesterday. “The second doses will be distributed a few weeks later to be in place for the second shot. These doses are being distributed at states’ direction to the American people as quickly as they are available and releasable, and the rapid availability and distribution of so many doses—with 20 million first doses allocated for distribution just 18 days after the first vaccine was granted emergency use authorization—is a testament to the success of Operation Warp Speed.”
It’s difficult to argue with that assessment when comparing the United States’ vaccine rollout to other nations’ around the world. In raw numbers, no country has administered more doses. On a per capita basis, only three—Israel, Bahrain, and the United Kingdom—have. Israel has already vaccinated more than 7 percent of its population.
Forman said the United States could be on that glide path too, if the process were more centralized. “When you’re dealing with a public good like a vaccine program, you count on the federal government,” he said. “You count on coordination in order to help facilitate the sort of things that you might not even be familiar with at the state level, as well as to be able to provide the funds, to be able to jumpstart something like this.”
In this regard, the Trump administration has erred more on the side of federalism. “The Federal Government has distributed the vaccines to the states,” President Trump tweeted yesterday. “Now it is up to the states to administer. Get moving!”
The Biden administration appears poised to take a more hands-on approach.
“I have directed my team to prepare a much more aggressive effort with more federal involvement and leadership to get things back on track,” Biden said this week. “This is going to be the greatest operational challenge we have ever faced as a nation, but we’re going to get it done. But it’s going to take a vast new effort that is not yet underway. … Vice President Harris and I have been speaking with county officials, mayors, and governors of both parties to speed up the distribution of the vaccine across the nation. We are planning a whole-of-government effort.”







Please note that we at The Dispatch hold ourselves, our work, and our commenters to a higher standard than other places on the internet. We welcome comments that foster genuine debate or discussion—including comments critical of us or our work—but responses that include ad hominem attacks on fellow Dispatch members or are intended to stoke fear and anger may be moderated.