After two months lived under the threat of coronavirus, the key characteristic of the crisis remains uncertainty. We don’t know where the virus came from. We still don’t know for sure all the ways it attacks the body, which is a big part of why we still don’t know how best to treat it. We certainly don’t know how to cure it. And as it spreads—despite our best efforts, among asymptomatic carriers and carriers not yet symptomatic and carriers who have no choice but to keep coming into contact with others—we still don’t know with nearly enough precision to whom exactly it has already spread.
On this last question, at least, we’d seemingly been making strong progress in recent days. After a rocky April, during which America’s COVID testing apparatus struggled to keep up with the demand of spiking cases, we righted the ship in May: According to official state data accumulated by the COVID Tracking Project, the last day we processed fewer than 200,000 tests was April 27, and we’ve averaged more than 350,000 a day over the last week. Over the past month, the percentage of new tests coming back positive—a key metric of how successfully our testing operation is growing relative to the growth of the pandemic itself—has gone from north of 20 percent down to a much more encouraging 5 percent to 6 percent.
We’ve known for a while there were blips in this data. On May 13, The Atlantic reported that the state of Virginia was fudging its testing numbers by combining the results of two incomparable types of tests in their official number: the PCR or nasal swab test, which determines whether a person is currently harboring the virus, and the serology blood test, which checks for COVID-fighting antibodies to determine whether a person has ever had the virus.
Serology tests are useful in many ways: People who are shown already to have had the virus can likely safely re-enter the workforce, and their donated plasma is among the most promising early treatments doctors have discovered for people still suffering from the virus. At the macro level, knowing what percentage of the population has already been exposed is a crucial factor in many public health decisions. But when it comes to the most pressing current reason for testing—knowing how many new cases are cropping up in a given region—they are useless.
Combining the two, therefore, is an extremely foolish strategy that seriously obscures the public health situation. After the fudging in Virginia was revealed, the government apologized and pledged to separate the data, and that seemed to be the end of it.
Only it turns out that this issue was far more widespread than anyone had previously thought. This week, we learned that not only Virginia, but also Pennsylvania, Texas, Georgia, Vermont, and Maine had been likewise combining their testing data. Meanwhile, the Centers for Disease Control had been doing the same thing at the national level—combining the two types of tests in their own state-by-state totals even in cases where states had reported them separately.
The news is a blow, one which casts serious doubt on the formerly encouraging testing numbers. What accounts for this extremely basic categorization error? In at least one state, the answer appears to have been politics of the “prisoner’s dilemma” variety.
“If another state is including serological tests, and they’re ranked above Virginia, and we are not, and we’re getting criticized for that, hey, you can’t win either way,” a top Virginia official told reporters earlier this month. “Now we are including them, and our ranking will be better, and we’re being criticized.”
The CDC’s decision to begin lumping the data this week has seemingly given the other states cover to fess up to the practice, too. In a statement, the Georgia Department of Public Health insisted that it was “following current Centers for Disease Control and Prevention methodology” in lumping the numbers together.
What’s less clear is why the CDC opted to do the same in the first place. While many have assumed that this, too, was a political decision designed to airbrush the federal pandemic response, it’s unclear that lumping all the nation’s PRC and serology tests together would actually lower the test-positivity rate overall.
In states that are still early on in their pandemic curves, lumping in serology tests drives down the rate dramatically. But in states like New York and New Jersey that have already crested the wave of new infections, lumping in serology tests would actually bump test-positivity higher, since so many people have already had the disease. As time goes on, and the ratio of people who have the disease compared to those who have had it continues to shrink, combining the data would serve less and less of a political purpose to anybody.
In other words, it’s an open question whether putting serology and PCR tests in the same data bucket actually makes the data look rosier. What’s undeniable is that it makes the data itself far, far worse.
“It’s horrible,” Dr. Howard Forman, a professor of public health at Yale, told The Dispatch. “It’s like the stupidest thing to do, and it doesn’t even serve any political end. I don’t even think that they’re doing it purposely to be deceptive. I think they’re being lazy.”
If there’s a silver lining here, it’s that this problem, now brought to light, shouldn’t be too difficult to rectify. Keeping these two dissimilar data sets separate statistically is the easiest thing in the world; all states and the CDC have to do is stop mixing them. Within a week or two, we’ll hopefully have a clear picture again of where our testing operation stands.
The bigger issue, Forman said, is how this debacle reflects on the reliability of the CDC and their aptness to handle the current crisis in general. For months, the CDC has done a subpar job tracking and publishing state testing numbers at all, largely ceding that collating work to outside outfits like the COVID Tracking Project. For them now to have flubbed such a foundational element of that work is not an encouraging sign.
“Let’s face it: The apparatus that you would have to put in place to have done this part of things really well is tiny,” Forman said. “It’s a less than a million-dollar-a-year operation, right? Four analysts with phones and a couple of higher-level associates tracking data from 50 states, telling them the deadline that they have to have for reporting data to you… I can’t for the life of me get my head wrapped around why we haven’t fixed something as simple as that.”
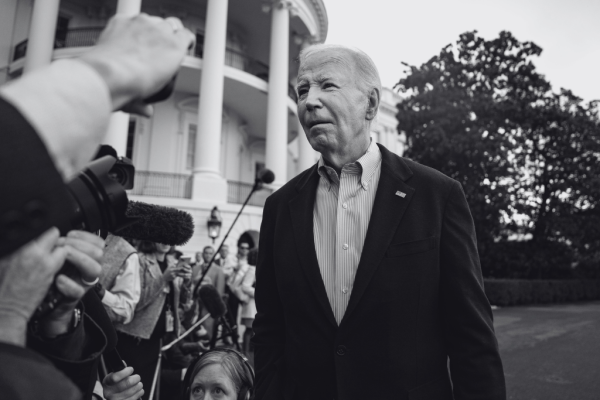
Photograph by Paul Hennessy/Echoes WIre/Barcroft Media/Getty Images.






Please note that we at The Dispatch hold ourselves, our work, and our commenters to a higher standard than other places on the internet. We welcome comments that foster genuine debate or discussion—including comments critical of us or our work—but responses that include ad hominem attacks on fellow Dispatch members or are intended to stoke fear and anger may be moderated.
You are currently using a limited time guest pass and do not have access to commenting. Consider subscribing to join the conversation.
With your membership, you only have the ability to comment on The Morning Dispatch articles. Consider upgrading to join the conversation everywhere.