Stopping the spread of the pandemic is in the hands of the people now. But what if the information about how to slow the spread authorities have been giving them for months is insufficient?
With cases spiking around the country, testing and tracing operations falling behind everywhere and getting completely snowed in where they’re needed most, and most states not considering re-entering lockdown, the primary factor that will determine whether things begin to improve or get even worse will be the conscientiousness of Americans in taking individual action to stop new infections.
The primary forms that action should take are the same as ever: maintaining social distance as much as possible, and wearing masks in public. But some scientists are growing worried that these two factors don’t present a complete picture of what reasonable steps should be taken to reduce viral spread.
The evidence is beginning to accumulate that the virus is transmitted from person to person via means that are subtly more different than we’d long assumed—with substantial ramifications for what everyday anti-viral precautions should entail.
In the early days of the pandemic, with bad news about the virus’s deadliness and contagiousness piling up every day, one reassuring data point stood out: At least this thing’s not airborne! “The virus that causes COVID-19 is mainly transmitted through droplets generated when an infected person coughs, sneezes, or speaks,” World Health Organization messaging maintained in March. “These droplets are too heavy to hang in the air. They quickly fall on floors or surfaces.” Frequently wash your hands, disinfect potentially contaminated surfaces, and stay at least six feet away from potential carriers, the conventional wisdom went then, and you’d be in good shape.
As early as May, we had discovered that half that prescription was wrong: The Centers for Disease Control announced that month that the virus did not spread easily via contaminated surfaces, reducing the ubiquitous “wash your hands” mantra from an anti-COVID battle cry into a simple piece of good-hygiene advice.
This summer, the evidence has been accumulating that the other half of that WHO guidance was wrong, too. It’s becoming clear that many of the droplets the virus attaches to are small and light enough to hang in the air for hours—and that these “aerosols,” as they’re called, are a significant contributor to the person-to-person infection driving the pandemic.
Earlier this month, 239 scientists in more than 30 countries sent an open letter to the WHO imploring them to update their guidance about the threat of airborne spread.
“Studies by the signatories and other scientists have demonstrated beyond any reasonable doubt that viruses are released during exhalation, talking, and coughing in microdroplets small enough to remain aloft in air and pose a risk of exposure at distances beyond one to two meters from an infected individual,” the letter reads. “Hand washing and social distancing are appropriate, but in our view, insufficient to provide protection from virus-carrying respiratory microdroplets released into the air by infected people.”
Last week, the global health body acknowledged the letter, telling reporters there was “evidence emerging” that the virus might linger in the air longer than originally thought.
Two major questions that have lately bedeviled COVID-watchers have been: Why do some people with coronavirus infect very few people, while others (so-called “superspreaders”) infect dozens? And why is the virus dramatically more contagious indoors than outdoors?
The scientists who signed the letter maintain that both phenomena can be most easily explained with reference to aerosols. If COVID is primarily transmitted via ballistic droplets—I breathe out, or yell, or sneeze, and fire off droplets that happen to hit your eyes, mouth, or nose before they hit the ground—then that should be able to happen outdoors as easily as in, and superspreader events would have to be attributed to really rotten ballistic luck.
If transmission takes place in large part via particles small enough to hang in the air, however, both superspreaders and increased indoor transmission risk make a great deal of sense. Two people six feet apart, no matter the setting, are largely safe from one another’s ballistic droplets. In addition to those droplets, however, each of them will also exhale a gradually growing and expanding cloud of aerosols, which given enough time in an unventilated room will spread throughout the space. If viruses can be carried by vapor that small, then the longer an infected person and uninfected people share the same space, the greater number of particles will be transmitted and the greater the infection risk grows. Give it enough time in a small enough space with enough other people around, and presto—you’ve got your superspreader event.
Outdoors, the slightest touch of a breeze will likely be enough to sweep those aerosols away, thinning the cloud until the particles are extremely unlikely to give anyone enough of a dose of the virus to make them sick.
Dr. Jose-Luis Jimenez, a chemistry professor at the University of Colorado-Boulder and aerosols researcher who signed the letter, explained the distinction with reference to smoke.
“If you’re smoking indoors, and you keep smoking, the entire place is going to look like a cloud,” he told The Dispatch. “If you smoke outdoors, the smoke follows the plume but goes away, and someone who’s 50 feet away or who passes you briefly may not smell the smoke.”
On the face of it, the fact that the coronavirus may be even more transmissible than previously thought is extremely lousy news. But the updated understanding also offers hope that the next round of social combat against COVID-19 may be more effective in arresting the spread than the current one has been.
What might that next round of combat look like? Well, for starters, we should keep doing the same stuff we’ve already been doing. The apparent presence of aerosol transmission doesn’t mean ballistic droplet transmission isn’t happening too, so judicious social distancing remains important. Regular hand-washing might not do much to defeat coronavirus, but it does battle a host of other diseases, and the less we have to worry about them the more we can focus medical resources on the pandemic. And wearing a mask helps cut down on the number of aerosols a person flings out as well as droplets—although with aerosols it becomes much more important to wear a mask that fits snugly across the nose and over the chin.
Other aerosol-avoiding considerations are new. When entering indoor public spaces, it would behoove a person to consider not only the distance they keep from others, but also the duration of their stay. A single puff smokes up a room a whole lot less than a whole cigar.
There are ramifications for those who sanitize and maintain public spaces too. Moving people through indoor spaces quickly can help prevent the accumulation of enough aerosols to infect others. Not for nothing are bars, where people tend to sit unmasked for extended periods of time, the face of the new spike in COVID cases. Unfortunately, there are ramifications here for larger gatherings like worship services too.
Efforts could be made to increase ventilation of indoor spaces as much as possible. The more virus-laden aerosols are ushered outdoors where they can’t hurt anybody, the better. Finally, buildings that make use of recirculated air might seriously consider equipping those systems with HEPA filters capable of trapping tiny particles like COVID aerosols.
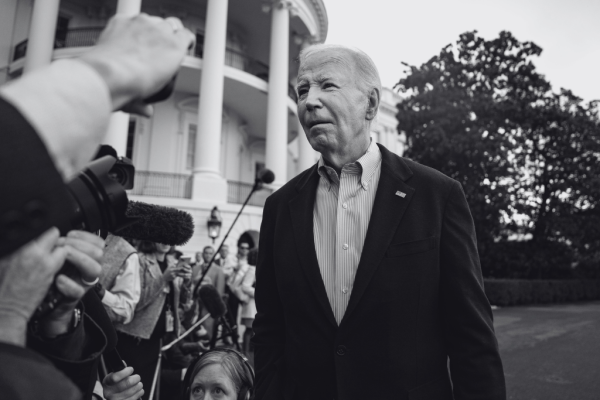
Photograph by Sean Gardner/Getty Images.






Please note that we at The Dispatch hold ourselves, our work, and our commenters to a higher standard than other places on the internet. We welcome comments that foster genuine debate or discussion—including comments critical of us or our work—but responses that include ad hominem attacks on fellow Dispatch members or are intended to stoke fear and anger may be moderated.
You are currently using a limited time guest pass and do not have access to commenting. Consider subscribing to join the conversation.
With your membership, you only have the ability to comment on The Morning Dispatch articles. Consider upgrading to join the conversation everywhere.